SIT Procedure Breakdown: How Does Selective Internal Radiation Work?
Liver cancer presents a challenge to treat and requires a complex multidisciplinary approach in order to achieve optimal results. Selective Internal Radiation Therapy (SIT), or radioembolization as it is also called, is emerging as one of the most promising treatments for patients with liver tumours. This innovative technique delivers targeted radiation to liver cancerous cells. It’s a less invasive alternative than traditional therapies. In this article, you will learn about the SIT treatment, its function, and the role it plays in the management of liver cancer.
Understanding Selective Internal Radiation Therapy
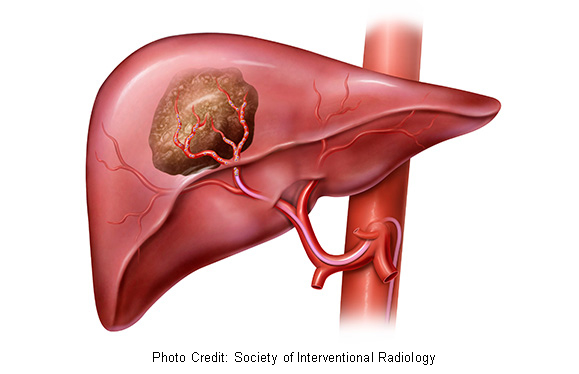
Selective Internal Radiation Therapy (SIT) is an effective form of targeted radiotherapy that can be used to treat cancerous liver tissue while minimizing any damage to healthy surrounding tissue. SIT delivers radioactive particles directly to the tumour blood vessels, unlike external beams of radiation that are delivered from the outside. This allows for precise radiation targeting of cancerous tissue within the liver without exposing normal tissue nearby.
SIT Procedure Process
SIT usually involves a series of steps that begin with a thorough evaluation of the patient to determine their suitability for the procedure. Before SIT is performed, patients will undergo imaging studies like CT scans or angiograms to evaluate the size, location, vascularity and extent of liver tumours. Once patients are eligible for SIT treatment, they will be scheduled for a plan session to develop the treatment strategy.
During a planning session, interventional radiologists use advanced imaging technologies to identify precisely the blood vessels that supply the tumour. This information helps determine the optimal placement of radioactive particles during the treatment. Once the treatment plans are finalized, patients can be scheduled to undergo the SIT procedure. This is normally performed in a specialized Interventional Radiology suite.
Benefits SIT procedure
SIT treatment for liver tumours offers several advantages compared to other traditional treatments. SIT has a unique approach to radiation therapy that is targeted. SIT, by using radioactive microspheres to target the tumour, minimizes the damage to healthy liver tissue.
SIT is also a minimally invasive procedure that can be done as an outpatient treatment in many cases. Compared to those who undergo more invasive surgeries, patients who undergo SIT will experience shorter hospital stays, faster healing times, and reduced discomfort following the procedure. SIT is thought to improve the quality of life in patients with liver tumours.
SIT also can be used in advanced liver disease patients to reduce symptoms and improve their quality of life. SIT is an extremely versatile treatment option for liver cancer. Individualized treatments can be tailored to meet the specific needs of each patient.
The Role And Responsibility Of Interventional Radiologists In SIT
Interventional radiologists play a crucial role in ensuring the success of SIT. These highly-trained physicians have received specialized training to use image-guided techniques for performing minimally invasive surgical procedures, including SIT. Interventional radiologists work closely with members of the healthcare staff, including radiation oncologists (RO), hepatologists (H), and oncologists, in order to create treatment plans and optimize outcomes.
Our team at https://www.asappaindocs.com/ is dedicated to providing high-quality care for liver cancer patients. Our experienced interventional radiologists use state-of-the-art technology and innovative treatment methods to deliver personalized, effective therapies.
Conclusion
Selective Internal Radiation Therapy (SIT) is an important advancement in treating liver cancer. SIT provides a targeted treatment that is minimally invasive. SIT is able to shrink tumours by avoiding healthy tissue and precisely targeting cancerous tissues within the liver. SIT is a comprehensive treatment that can be tailored to the individual patient’s needs. With the help of an interventional team and multidisciplinary support, SIT can provide compassionate and comprehensive care. SIT remains an effective tool in fighting liver cancer as the field evolves. It offers patients and families hope for a better future.





